The results of my genetic test arrived in an unpretentious white envelope.
It was the summer of 2021, and I almost missed it when I flipped through the mail, but I set it aside from the rest of the bills to look at later. About a month before, I had sent a sample of my saliva to a genetic testing company in California. I wasn’t even nervous about opening it, so sure was I that it wouldn’t be a big deal.
Looking back on it now, it seems wildly naïve.
At that point, my family and I had already weathered a grueling three years dealing with the fallout from a cancer diagnosis. In 2018, we found out that my mom, Teresa, had stage 4 ovarian cancer. The diagnosis was sudden, preceded by six months of uncertain and confusing symptoms like back pain, bloating, and loss of appetite. And then there was the shock of stage 4 cancer: Right off the bat? Wait, how many stages are there? My mind reeled as I immediately googled it. I didn’t even have a basic knowledge of ovarian cancer at the time.
I stopped doing those internet searches pretty quickly; all I found were grim statistics and websites so dense with scientific jargon I could barely find the verb in a sentence. What I could understand was that ovarian cancer, not as well known or well funded as breast cancer with its ubiquitous pink ribbon, is the deadliest gynecological cancer there is.
There is no way to screen for this disease, unlike breast or cervical cancer, with their annual, routine tests—mammograms and Pap smears. So we often can’t see ovarian cancer in its early stages, which is one reason why it’s so deadly.
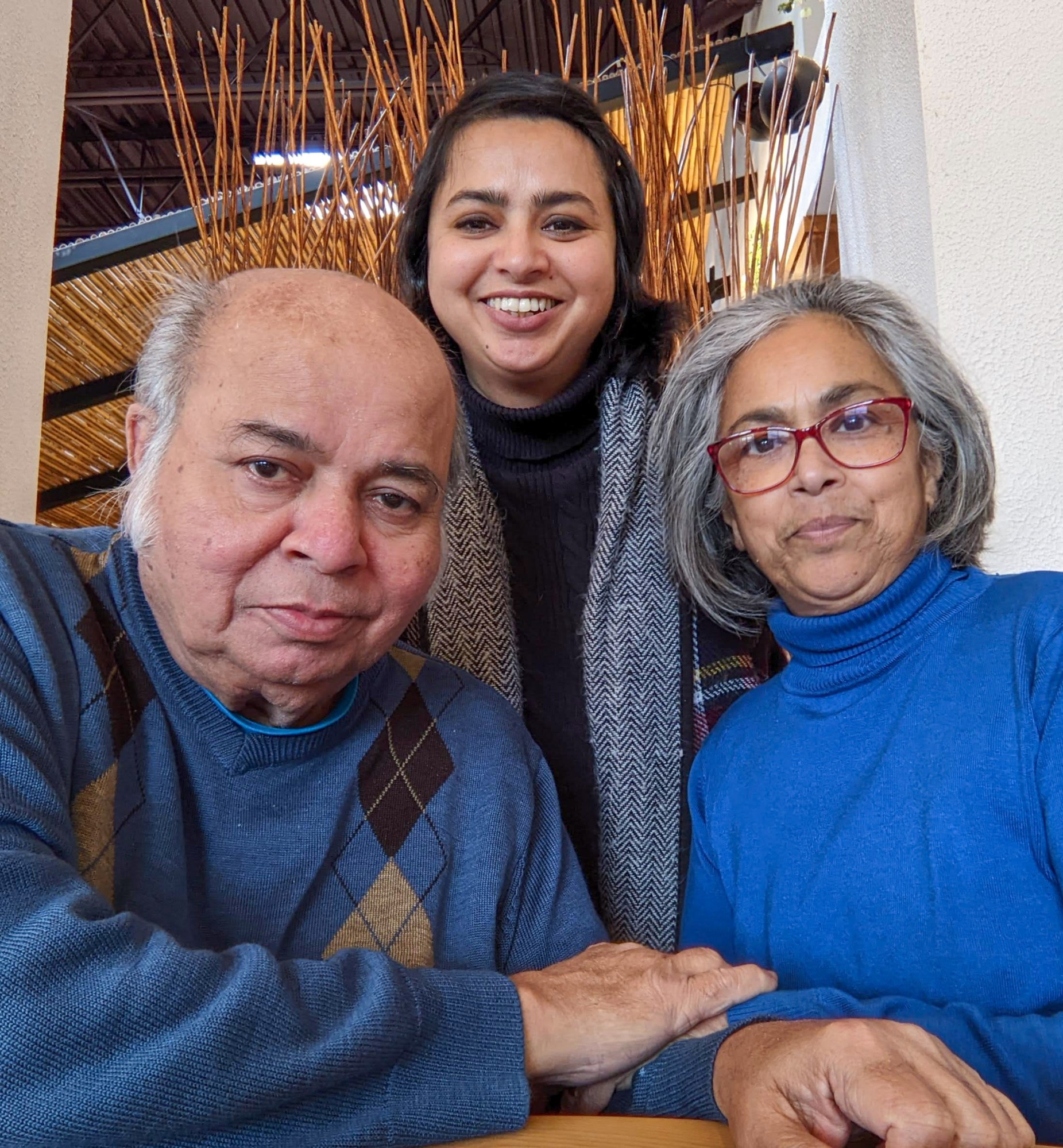
The odds were stacked against her, but my mom somehow survived after a brutal six months of chemotherapy. The relief was palpable for my family. When she was well again, in early 2019, she celebrated with a kids-and-grandkids tour, since my brother, sister, and I are spread out across different countries. She started to try to live life normally once more.
When the cancer came back 11 months later, the rug was pulled out from under us again, and we were distraught, shocked.
The doctors, however, were not.
I found out later that the way my mom’s cancer presented was textbook: vague symptoms, a surprise diagnosis, and eventually a recurrence, which happens in 70 to 95% of people who were initially diagnosed with ovarian cancer in stages 3 or 4. This is how the disease goes, for the most part.
After that first recurrence, doctors recommended that my mom do a genetic test, accompanied by genetic counseling.
Mom’s results came back positive for a gene mutation, which had contributed to the development of her cancer. This aberration is in a gene called RAD51C. When she found out, her first action was to call her kids—all three of us—and urge us to go get tested ourselves. It was important and urgent that we do this, she said, because this was the best—and probably only—way to prevent us from being vulnerable to this cancer too.
That’s why, eventually, I did get tested: I sent off that little sample to the lab, and received that envelope in the mail.
But opening it and reading the results—which revealed that I was a carrier of this mutation also—took me down a path I would never have imagined traveling. I’ll shortly have surgery for prophylactic removal of my ovaries and my fallopian tubes, as a way to make sure I don’t go through what my mom has gone through: four rounds with this cancer in the last five years.
In some ways, things are looking up, strange though that may sound for a disease with such a grim survival rate. Scientific advances now offer more opportunities for treatment and prevention than ever before. Increasingly accessible and affordable genetic testing has provided a huge step forward for dealing with a cancer for which there is no screening tool, and whose mortality rates have remained stubbornly high for the past several decades. This is, finally, a way to see around the corner to some extent, a new reason to allow some hope into the conversation.
At the same time, recent discoveries have shown that the most common and deadliest form of ovarian cancer starts not in the ovaries but in the fallopian tubes, and that ovarian cancer is not even one cancer but comprises several distinct subtypes.
This has all informed a new recommended course of action for “high-risk” people like me. Though it may seem like an extreme step, removing both tubes (a salpingectomy) and ovaries (an oophorectomy) is at least something an individual can do to manage the risk.
But on a personal level, it’s a hard, anxiety-inducing decision to make. Removing the ovaries leads to immediate menopause, which is not just a giant change in any woman’s life but also increases the risk of cardiovascular disease, dementia, and stroke. Now that I know exactly how important these hidden and underrated organs are, I’m reluctant to part with them, frankly. But there’s no getting away from those grim statistics—most women who get ovarian cancer die from it. So removing my ovaries and fallopian tubes is not an ideal plan of action—but it’s the only one we’ve got so far.
Now an (ever so slightly less) overlooked cancer
When my mom was first diagnosed, I asked her to start recording audio diaries on her phone to document her experiences, whether good or bad. Maybe we can do something with it one day, I told her. Now, five years later, I finally have: “Overlooked: A Podcast about Ovarian Cancer” charts my family’s journey in 10 episodes and explores how little we knew about this disease for many, many years.
“I think the ovaries might have suffered a little bit from paternalistic, misogynistic practices of the past. I think we only really, in the last 20 to 30 years, have come to realize how important the ovaries are.”
I started gathering content for the podcast way before anybody mentioned genetics. This was meant to be a story about my mom, her journey with this cancer, and what it could teach the rest of us.
At the time I wasn’t thinking about my own part in this story. I reluctantly became part of it, though, when I did that genetic test.
Just in the last few years, new scientific discoveries and more widespread genetic testing have really driven a change of approach in treatment and prevention of all sorts of diseases and ovarian cancer specifically—stories that I covered for the show. This disease is now ever so slightly less overlooked than it used to be.
Nevertheless, it’s critical to understand why it was largely ignored for so long.
The most fundamental and chilling reason came from Emilie Chiasson, my first interviewee in 2018, who was at the time an advocate with Ovarian Cancer Canada, an organization that raises funds and works with researchers and patients. She told me about the phrases people used to describe this disease, referencing its stealthy nature—“the silent killer” and “the disease that whispers.”
And then, she hit me with the stark reality: “Why don’t we know more about this? Well, because unfortunately, most people that are affected by the disease sadly die as a result of it and/or they’re very sick” by the time they’re diagnosed.
“So they’re not out there advocating, marching on [Canada’s Parliament] Hill, wearing pink, doing all the things that women have done to really move forward [on] breast cancer,” Chiasson added.
My own theory, though, has more to do with how we’ve regarded the ovaries historically. As Dianne Miller, a pioneering gynecological oncologist in British Columbia and cofounder of OVCARE, a multidisciplinary research program there, told me, “I think the ovaries might have suffered a little bit from paternalistic, misogynistic practices of the past. I think we only really, in the last 20 to 30 years, have come to realize how important the ovaries are.”
Important—and complex.
In the process of producing the podcast, I learned that the ovaries play a hugely significant role in a woman’s health beyond fertility or even menstruation and menopause. They have an impact on cardiovascular disease, Alzheimer’s, osteoporosis, and more.
The term “ovarian cancer” is not even as straightforward as it sounds, being an umbrella term for different cancers. Doctors only figured this out in 2008, and it was “a huge step forward,” says David Huntsman, the director and another cofounder of OVCARE, whose work was critical to understanding the spectrum of ovarian cancers. The most common—and lethal—type is epithelial ovarian cancer, of which there are several subtypes; they form in the tissue surrounding the ovary, or in the lining of the fallopian tubes, or in peritoneum. There are also germ cell tumors and ovarian stromal tumors, which are rarer.
The treatment to some extent depends on the subtype—or at least it should. Previously, Huntsman says, “we were treating a kind of mixture of different problems and trying to find a solution which was going to fit across them, which was never going to work.”
My mom’s subtype was an epithelial cancer called high-grade serous, and her first round of treatment was three sessions of chemotherapy; then a “debulking” surgery to remove the cancer and all the reproductive organs; and then three more sessions of chemotherapy.
But while doctors understand the cancer better these days, there’s still no way to see it coming: a recent major study in the UK showed that there is no solid way to screen for it. The closest we’ve come is a blood test for a marker called cancer antigen 125, but it’s far from a fail-safe test. CA125 is sometimes elevated in a person with ovarian cancer. But there are other causes of a high CA125 (like endometriosis, for example), so doctors don’t consider this a reliable indication of cancer.
Making matters worse, ovarian cancer symptoms are dangerously vague: feeling bloated or full after eating very little, or sometimes experiencing pain in the pelvis or the back. These are all easily and often misattributed to other health issues. For years, ovarian cancer advocacy organizations have run campaigns to increase symptom awareness in an effort to detect this cancer early. Yet at the same time, in the words of one of my mom’s oncologists, the disease has been “outsmarting” us.
Educating primary-care doctors, who are often the first type of health-care provider that women see about their symptoms, is an important element in tackling the problem of how to spot this cancer.
Organizations like Target Ovarian Cancer in the UK have been working for several years to increase awareness of symptoms among primary-care providers within the UK’s National Health Service. But from a physician’s point of view, ovarian cancer won’t be the first thing they think of as they sift through broad symptoms like bloating and pelvic pain—something I heard not just from advocacy organizations, like the UK group, but also from researchers and oncologists in the US and Canada who have worked with physicians. The bottom line is that it’s just a tough cancer to diagnose early.
This all adds up to a bleak reality: the cancer is mostly caught in later stages, when it has already spread and is difficult to treat. That’s why genetic testing has become the most important preventive tool there is, particularly since about 20% of cases are hereditary. (Hereditary cancers also have a higher recurrence rate.)
Knowing your genetic make-up, and whether your body carries a gene mutation that makes you susceptible to a certain type of cancer, is empowering. But with that knowledge comes a new, tough set of decisions.
A genetic puzzle
If a genetic mutation could become a household name, it kind of happened when, in 2013, Angelina Jolie had a bilateral mastectomy after finding out she was a carrier of a mutation in the BRCA1 gene. Mutations in BRCA1 and BRCA2, discovered about 30 years ago, can increase the risk of breast cancer by up to 85% and of ovarian cancer by up to 60%.
The mutation my family has is less well known, more newly discovered, and rarer. But the RAD51C mutation also means I have a genetic predisposition to ovarian cancer, and potentially breast cancer too. The risk—currently 10% for me—increases with age until about 60, when it starts to decrease.
When my mom first called me with the results of her genetic test, she sent me the report. My eyes glazed over. It was hard enough to deal with the fact that she was sick again and would go back to chemotherapy soon. But now I would also have to wrap my brain around understanding this complicated genetic mutation. The idea of “mutations” took my lizard brain straight to X-Men.
My mom and I have this inside joke about how science teachers (her) struggle to explain “science-y” things to liberal arts majors (me), and after she had finished reading me the details of her report, there was a pause on the call. “Explain it to me like I’m a liberal arts major, Mum,” I said.
The RAD51C gene is what’s called a “susceptibility gene,” meaning it’s supposed to protect the body from certain cancers, and a mutation means it can’t perform this job. In this case, that means fighting ovarian cancer.
All three of us siblings have made different choices about testing. My brother has not yet been tested but plans to, because as a carrier of this gene, he could pass it on to his kids. My sister did hers almost straight away—the trauma of watching Mom go through that first round with cancer motivated her to react quickly. She found out she too has the mutation.
The same fear that compelled my sister to act kept me frozen in hesitation and reluctant to open what I knew would be a Pandora’s box. Around that time the pandemic hit anyway, and everything to do with health care became laser-focused on covid-19; I put off getting myself tested until early 2021.
I later got in touch with the San Francisco–based genetic testing company Invitae to get an overall picture of how testing is working within the realm of ovarian cancer. Ed Esplin, a clinical geneticist there, told me that although more people are being tested for this disease and for others, it’s still not systematic.
“Unfortunately, there is evidence that less than 40% of all of the cancer patients who already qualify—according to the clinical practice guidelines for genetic testing—are actually getting it, which is a travesty, in my personal opinion,” he says.
But last summer Esplin coauthored a paper published in the Journal of the American Medical Association showing that rates of testing for patients diagnosed with ovarian cancer are growing: back in 2013, fewer than 30% got a genetic test; by 2019, that share was more than 40%. Nonwhite patients were tested less frequently, but their rates were also increasing.
Testing can inform every aspect of a cancer patient’s care, but the key is that it needs to be done early. “Part of what that’s going to take is education of physicians and patients,” Esplin adds, “so that they understand how critically important genetic testing is, so that it gets done. Part of that is going to be health-care institutions in which these physicians are practicing, putting into place workflows that make this automatic.”
My family’s experience is again an example of how this is just beginning to take root: my mom was asked to do a genetic test the second time her cancer was diagnosed, not the first time. Testing is not in any way “automatic,” but there’s certainly more discussion about it than there used to be, even a mere five years ago.
Once I finally decided I’d put it off long enough, the process to get tested started with an initial session with a genetic counselor—in my case, a two-hour deep dive into everything from family history with cancer to the nature of my monthly cycle. Then I paid $250 out of pocket for my test, which wasn’t covered by my insurance provider, and sent my saliva to Invitae. That price tag puts it out of reach of a lot of people, but the price of testing has actually fallen dramatically in the last 20 years, which makes it much more accessible to the wider public than it used to be.
While I probably should have anticipated what my test would reveal, given that my mom and sister were both positive, the result still caught me off guard.
I had convinced myself that because this was a “rare” mutation, as all the literature had labeled it, I might not have it. But that was a function of the fear that had gripped me for the previous two years; my intellectual understanding of this disease was filtered through a highly emotional lens, and my brain didn’t want to accept what the implications were.
I can now understand why people might not want to put themselves forward for testing: there’s no turning away from the knowledge once you have it, and a positive result does force a decision on what to do next.
A radical treatment plan
The discovery some 15 years ago that most ovarian cancers start in the fallopian tubes has radically changed how patients—and even women who don’t know if they may be at risk—are treated.
Miller, the gynecological oncologist from British Columbia, is now retired but led a team at Vancouver General Hospital that is credited with this discovery—as well as with a new approach of removing the fallopian tubes preventively.
So when we spoke, I started out with a cheeky question designed to provoke: “I’m shortly going to have my fallopian tubes out. Do I have you to thank for that, Dr. Miller?”
Without skipping a beat, she answered, “Probably not—I’m not your surgeon.”
Nevertheless, it was Miller’s team that rewrote the textbooks on where the most common and lethal type of ovarian cancer originates, and their work has now been turned into guidelines for diagnosis and care.
Their radical idea was “opportunistic salpingectomy”—removing the fallopian tubes altogether in any woman already having pelvic surgery, thus preventing ovarian cancer whether or not there was a known risk. (While drastic, this wasn’t, of course, the first time prophylactic surgery had been proposed for cancer prevention, since mastectomies are performed to similarly protect those susceptible to breast cancer.)
“Roughly a quarter of women in their lifetime will have their uterus taken out,” says Miller. In fact, hysterectomy is the second most common surgery for women in the US, often performed because of fibroids, endometriosis, cancer prevention, or uterine prolapse. “And if you think of that, if you could prevent a quarter of the high-grade serous cancers from occurring simply by making a slight modification to a surgery, that’s big—that’s better than any chemotherapy drug that’s been developed throughout my career.”
Miller’s team started doing this work in British Columbia around 2010, and since then they’ve done numerous studies to prove the safety and efficacy of salpingectomies. There are now 14 gynecological societies across the world, including the American College of Obstetricians and Gynecologists, that recommend opportunistic salpingectomies, and uptake has increased in Canada and the United States.
Gillian Hanley, an associate professor in the Department of Obstetrics and Gynecology at the University of British Columbia, says that only 8% of hysterectomies performed in the province in 2008 included an opportunistic salpingectomy; in 2019, 80% did.
Hanley also works with OVCARE, the research program cofounded by Miller, Huntsman, and another doctor; she says the organization has worked with physicians for years, and more recently with surgeons, to ensure that any woman who has a scheduled pelvic surgery is able to have a discussion about this preventive step.
“So if a woman is having a surgery, and she no longer wants any future pregnancies, there should be a discussion to say, ‘Hey, we’re in your pelvis. We can remove your fallopian tubes at the same time and dramatically reduce your risk for ovarian cancer. Is this something you would like?’” Hanley says.
This conversation obviously forces a decision, if one hasn’t already been made, about one’s desire to have or have more children. My sister, who found out two years earlier than I did that she’d tested positive for the RAD51C gene mutation, was 37 years old when she had her salpingectomy. She has two daughters and had decided that she was done having children, so the idea of removing her fallopian tubes was one she could live with. And having seen the toll this disease had taken on our mom, she wanted to get out of the line of sight of this cancer. When her daughters are older, they’ll get tested for this mutation as well.
These ideas have recently started filtering through to the wider public. Earlier this year, the US-based Ovarian Cancer Research Alliance, one of the largest advocacy organizations for this cancer, had a major shift from an emphasis on early detection; it is now recommending genetic testing, both for diagnosed patients and for other people who know they’re at risk. It now also counsels prophylactic organ removal: opportunistic salpingectomy for anyone at even “average” risk for the cancer; or, if you’re at increased risk, a salpingectomy whether or not it coincides with another procedure, as well as removal of the ovaries.
But this emphasis on genetic testing as a preventive measure hasn’t necessarily been welcomed across the ovarian cancer community, says Sarah DeFeo, the chief program officer at the Ovarian Cancer Research Alliance. “There is this strong attachment to the importance of symptom awareness. And there is this real focus on the promise of early detection,” she says. “And we know that does not work.”
“We need to focus on what does work and what we can do,” she adds. “And we encourage people to know their risk.”
What prevention really looks like
As for me, after I got my test results, I dragged my heels on a decision. After seeing the genetic counselor, I eventually found my way to a gynecological oncologist at New York–Presbyterian. There, I was told that the recommendation for high-risk women my age—approaching 50—is to have the ovaries as well as the fallopian tubes removed as a preventive measure.
This week, shortly before my 49th birthday, I’ll have this surgery, which will instantly trigger menopause—“surgical” or “forced” menopause are the correct and depressing terms. It fills me with dread, frankly. In an effort to prepare, I find myself going back to googling “what to expect,” and the list is astonishing: menopause can bring hot flashes, brittle bones, heart palpitations, memory loss, insomnia, joint pain, depression, vaginal discomfort, bladder issues, hair loss … I usually don’t make it all the way to the end of these lists.
This is where we’re at: a huge advance—finally—in science and technology has shined light on a cancer that has long been in the dark, and has been outsmarting us this entire time. But prevention comes at a price. I’m going to be a walking example of prevention very soon, and it does make me wonder: if you have a gene mutation like mine, it seems that the best way to not get ovarian cancer … is to not have ovaries (or fallopian tubes) at all, which tells me a lot about how powerful this disease really is.
I put that to Miller, who has spent the better part of her career with a full awareness of the disease she was trying to outsmart as a scientist. “I can’t disagree with you,” she replied. “But it’s really the best we have for right now. Is it perfect? Absolutely not, for exactly the reasons that you said. But on the other hand, having watched too many women die of ovarian cancer over my career, I just think we have to do something. And there’s something we can do without increasing the morbidity to women.”
So even as I turn back to googling, there comes a point when I remind myself that surgical menopause is a better outcome than even the possibility of ovarian cancer. It doesn’t take prisoners, this cancer.
Golda Arthur is an audio journalist and podcast producer. She has launched and run podcasts at Vox Media, MIT Technology Review, and Marketplace, and has reported, edited, and produced for the BBC and the CBC. She lives in New York City.
Comments
Post a Comment